If you follow me on my social media channels, then you already know this. In fact, our daughter is now 9 months old! She is starting to stand up by herself and babble and getting closer to walking.
Time flies.
The purpose of this post is not really to announce having a baby, but how we managed having another child while having our Type 1 daughter at home.
Not How we Planned the Gender Reveal
This all starts out when we were planning on how we were going to do a gender reveal. Spoiler alert – I don’t like gender reveal parties, but that’s a different conversation.
We decided to just do cupcakes with pink or blue filling on the inside. We were supposed to find out the gender on Valentine’s Day 2019.
Well, something happened on February 12, 2019.
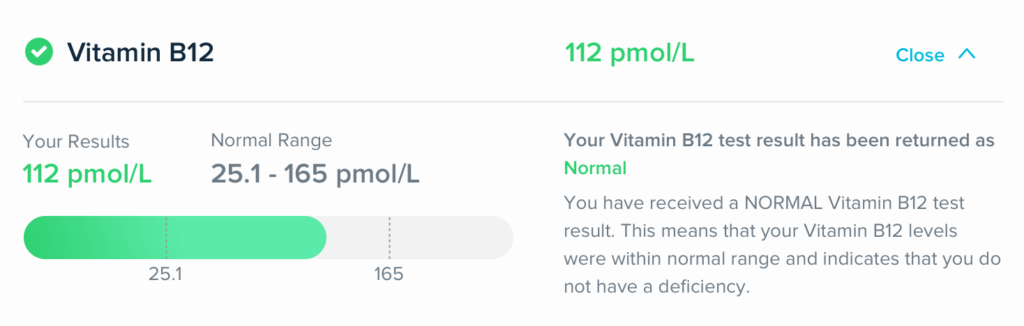
That was the morning of not only a major snow storm in northeast Pennsylvania, but it was the day our oldest daughter was diagnosed with Type 1 Diabetes.
We spent 2.5 days in the hospital, but on the second day, our appointment to find out the gender of our baby was actually in the same exact hospital that we were in for our daughter.
My wife and my mother (who was visiting at the time) went to the appointment while I stayed back with our daughter.
This was not really the way that we had planned on finding out the gender and doing the reveal to ourselves and friends and family. We decided to postpone the reveal until we got home from the hospital, so that’s what we did.
When we left the hospital the first day, it was past dinner time, so we didn’t want to rush it. So, we waited until the next day for my sister-in-law to bake cupcakes.
It’s a…
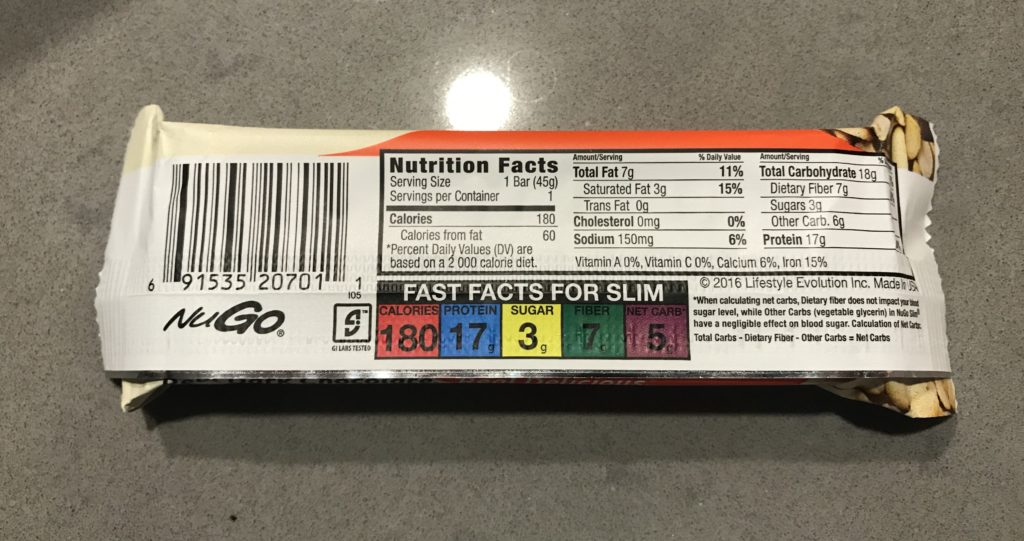
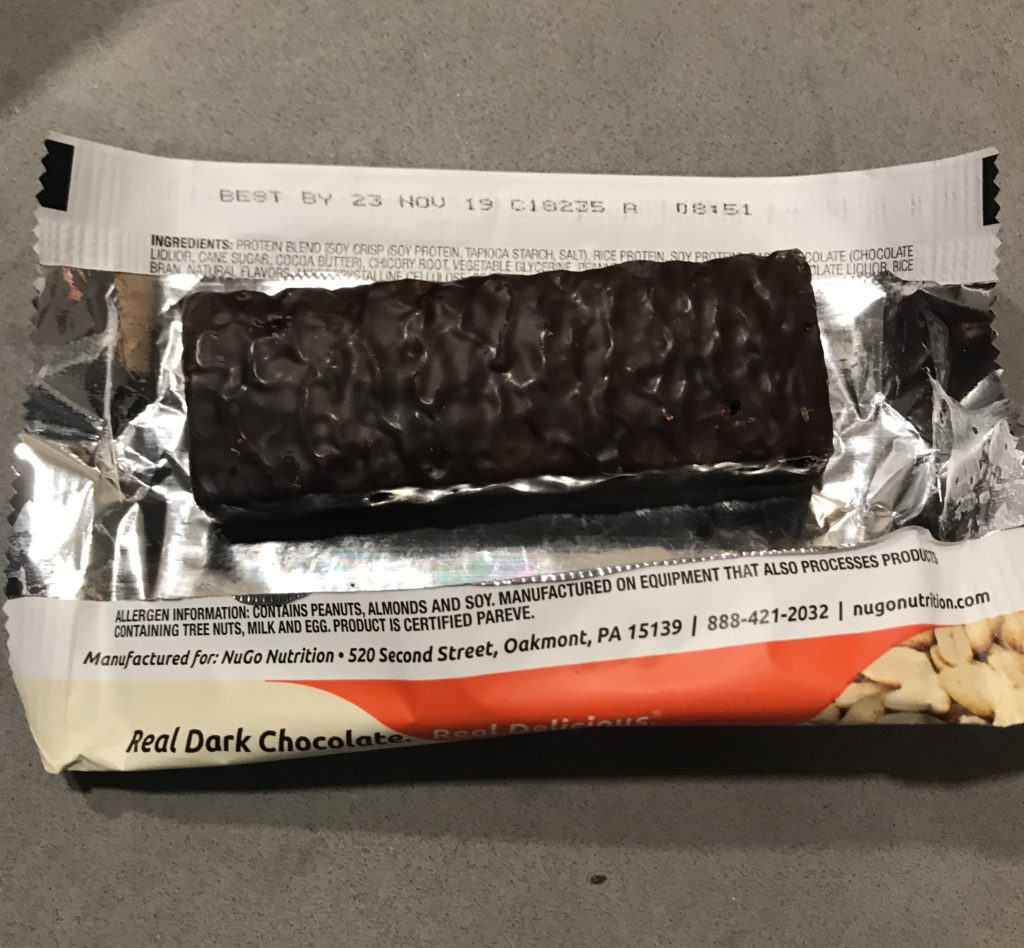
This was also the first time our daughter was going to have cupcakes as a person with type 1 diabetes (and it definitely wasn’t her last).
Surprise – it was pink inside!
Stress Started to Kick In
The next few months we were just adjusting to life with Type 1 Diabetes and learning strategies to deal with stress. My wife was pregnant and I was constantly concerned how her new stress levels were going to be affecting her pregnancy…this led to my higher levels of stress.
The stress really started to increase the closer we came to the due date.
What are we going to do with our daughter?
Who is going to give her the nightly basal?
Who is going to count her carbs?
Who is going to give her the bolus?
Who is going to check her blood sugar?
What are we going to do?
These questions went through our mind about 100 different times a day.
Time to Make a Plan
That’s when we sat down and made a plan. Obviously, this is a pregnancy and birth of a child, it’s unpredictable, but we were going to do our best to try and plan.
We had a few different plans in place. One for each time of the day that we had to go to the hospital when my wife was going into labor.
Our preference was her to give birth in the middle of the night. This would mean that I could possibly give our daughter her basal insulin shot and then get her to bed and then my parents could just sleep at our house and keep an eye on her Dexcom.
Then, I could go home in the morning and give her breakfast and a bolus shot and then get back to the hospital.
Our best plan almost came to fruition, it was very close.
How did it all happen?
My mother-in-law was flying in for my wife’s birthday and to also try and time the birth of our new daughter. My MIL flew in the afternoon of my wife’s birthday. My wife decided to stay home and not go to the airport because she was feeling some contractions and feeling a little “off”.
We ordered some pizza for dinner and started our daughter on her dinner.
And then that’s when my wife said, “it’s time to go to the hospital”
Wait, it’s my wife’s birthday, her mother just flew in hours ago, it’s getting towards night time (our perfect plan)…. is this really happening?
Oh yeah, it was!
Once my parents came to our house, my wife, MIL and myself left for the hospital.
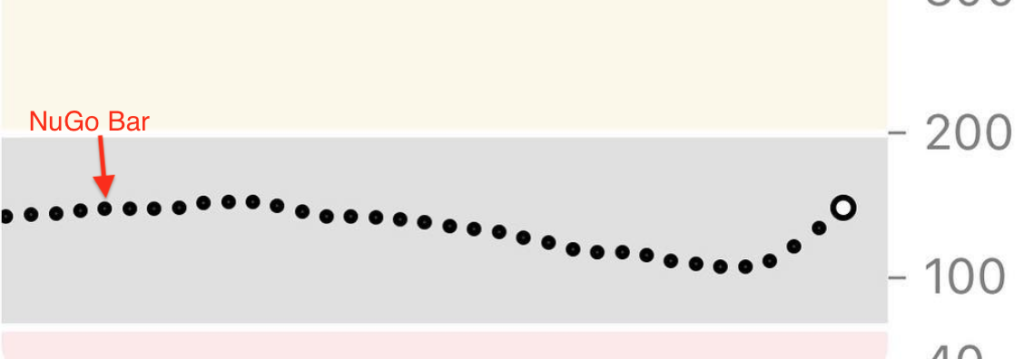
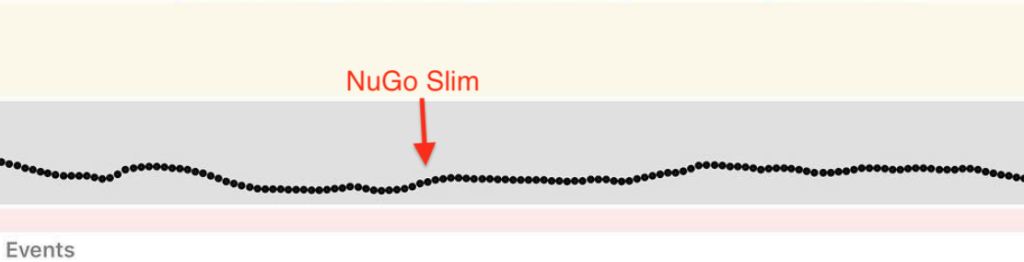
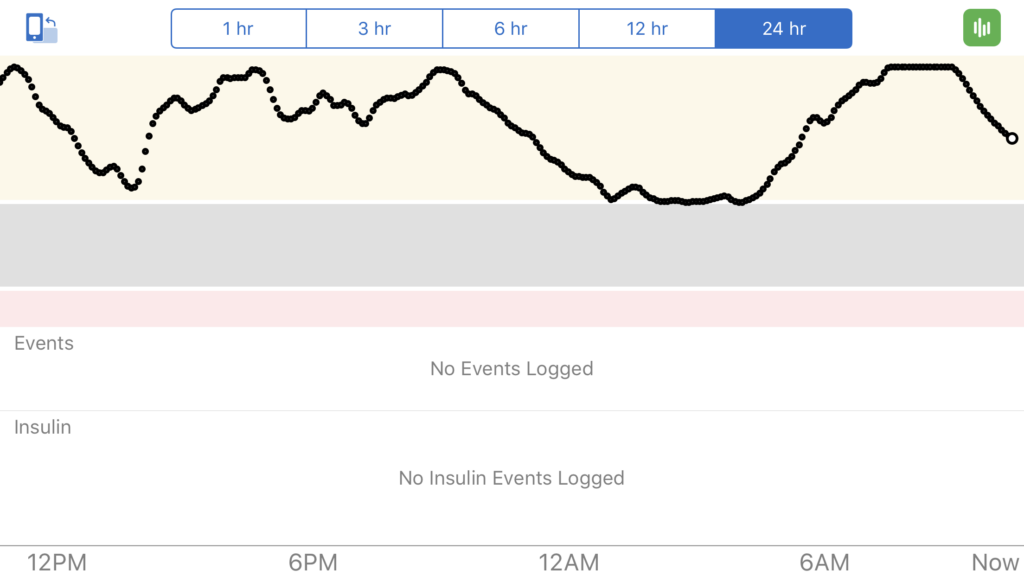
I’m going to fast forward through the rest of the labor and delivery, but while my wife was in active labor, I was checking my phone to see my daughter’s Dexcom numbers.
My sister-in-law came over to give her the nighttime basal shot. We chose this because my niece also lives with type 1 diabetes, so we trusted her decision making on diabetes. She’s seen needles, pen needles, meters, blood, etc.
Everything was going smooth. Her blood sugars were great while she was sleeping.
After Birth
After our second daughter was born, I was able to hold her and spend some time with her and also my wife who was recovering from delivery. My MIL was also there to be by her side which helped tremendously.
With my MIL being there, it allowed me to drive home at about 3 am to be home for my daughter. My parents stayed the rest of the night and morning, but it allowed me to get her breakfast ready and give her the breakfast shot and get her day started.
She was super excited to go and meet her new sister, so I brought her to the hospital with me.
From there, it became a little easier. She was with us at the hospital for most of the time. I hated leaving my wife and new daughter at the hospital, but she was never alone. Her mother was there when I would go home with our oldest daughter.
I’m not going to lie, this was very stressful trying to figure out how we were going to leave our 4-year old with Type 1 Diabetes with someone else for the first time, but also at the same time, enjoy the birth of our newest addition to our family.
It all worked out.
So, now, we are (well have been for 9 months now) a family of four. I am officially a 2X #girldad.