A recent study from the Kaiser Family Foundation reported in Becker’s Hospital Review breaks down how many patients in each state skip a physician visit due to cost.
I always like to look at these lists to see the top states and bottom states on these lists and think about maybe why these particular states are where they are.
In this particular case, my mind went a different way with this. My mind went to the idea of what happens when these patients skip visits.
Something that Victor Montori writes about in his book, Why We Revolt is that some times patients can’t afford a visit or just can’t make a visit for a specific reason and then that patient is deemed to be non-compliant.
The word non-compliant is a whole other issue and people like Renza can go into more detail on why language matters, but for this post, I will use that phrase.
Let’s say that I might be the most compliant, best patient out there and eager to do what I need to do in order to have a better doctor visit than the last one. So, that means I ate better, I exercised, I got better sleep and I took all the meds I was supposed to take.
But, unfortunately, I had a client become late on a payment and I had to fork out some money for some other non-health related emergency and next thing you know, I can’t afford my co-pay or other out of pocket expenses to go see my doctor.
Now, I look like a bad patient. My health potentially gets worse because I’m not able to review the lab results until I can afford to go see my doctor. But now, I have even more medications and tests that need to be done the next time, causing me to have even less and less money to afford future appointments.
Next thing you know, I’m being admitted to the hospital for poor health all because I couldn’t afford to go see a doctor.
Now, this exact situation hasn’t happened to me, per say, but it happens every single day.
Why These States?
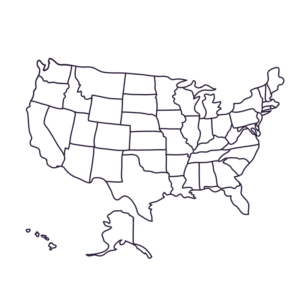
 What are the reasons behind why people in Texas, Mississippi, Louisiana, Georgie and Nevada to round out the top 5 can’t afford to visit their doctor?
What are the reasons behind why people in Texas, Mississippi, Louisiana, Georgie and Nevada to round out the top 5 can’t afford to visit their doctor?
Is it due to just overall struggling economies in those states?
Is it because of poor insurance coverage from Marketplace plans in those states?
Why do people in Iowa, North Dakota, Hawaii, Vermont and Massachusetts all have a far less harder time affording to go see their doctors?
These are questions that I always wonder when I see these lists.
I, for one, am glad to see that PA is 9th from the bottom of the list.
Share this article on Facebook or Twitter now and keep the conversation going.
Like what you read? Then sign up for The Life of a Diabetic newsletter to get all the week’s posts delivered directly to your email every Saturday morning.




 What are the reasons behind why people in Texas, Mississippi, Louisiana, Georgie and Nevada to round out the top 5 can’t afford to visit their doctor?
What are the reasons behind why people in Texas, Mississippi, Louisiana, Georgie and Nevada to round out the top 5 can’t afford to visit their doctor?