Yesterday, I wrote about our decision to start using an insulin pump as opposed to multiple daily injections. If you would like to learn more about why we made that particular decision, please go check out yesterday’s post.
Once we knew that we wanted her to be on an insulin pump, we needed to figure out which one. I pretty much already had an idea which one we were leaning towards.
We had a few options to choose from:
- Medtronic
- Tandem
- Omnipod
Medtronic
I personally used a Medtronic for 13 of my 16 years with diabetes. It was the first pump that I started on in December 2004 after my diagnosis in April of 2004 (couple days away from 16 years since diagnosis).
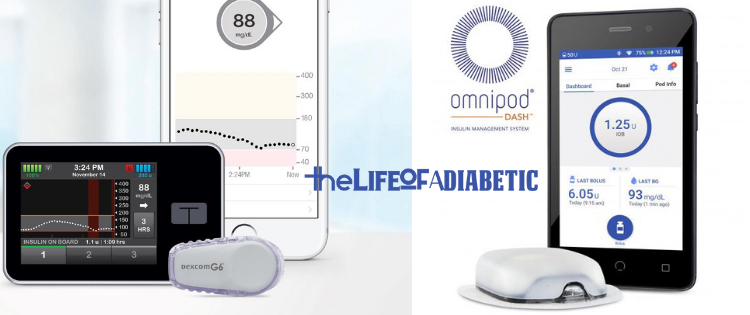
I was very comfortable with the Medtronic insulin pump and how it worked and how to use it. I also liked their low suspend technology that could detect a low blood sugar coming on and automatically shut the insulin delivery off.
However, that would require using their CGM, and I wrote last week about our reasoning for choosing Dexcom immediately for our CGM of choice.
The last, main reason, was I know our daughter. I know she runs around a lot and also bumps into plenty of things. I have also walked past a door and got my tubing snagged and had an infusion set rip out, and let me tell you…. it hurts!
Tubing was a no-go for us.
Tandem
Even though Tandem has tubing, it is integrated with Dexcom and offers their Basal-IQ technology, which was pretty appealing to me. If you’re not sure what technology I am talking about, you can check out an old post I wrote on it (and I’m also going to link to their site because they have had a bunch of updates since I last wrote about it).
In the end, we just knew we needed something without tubing.
So, that led to the choice of Omnipod.
Omnipod
After my 13 years with Medtronic, I chose to use MDI for a year. It worked out pretty well for me. I wrote about my decision to give up an insulin pump for MDI in the past.
When I decided that I was done with MDI (again), I wanted to go back onto an insulin pump, but I felt like it was time to give up Medtronic. Primarily because I switched over to Dexcom during my year of MDI.
I decided to use an Omnipod.
I tell you that story, to further explain why we chose Omnipod.
90% of the decision was because of it not having any tubing. It was a pretty clear cut decision for us to make.
90% of the decision was because of it not having any tubing. It was a pretty clear cut decision for us to make. Click To TweetThe remaining 10% was a little bit of the fact that I currently used (and still use) asn Omnipod, so there was the comfort level of knowing how to troubleshoot it if needed.
Daddy, Daughter Diabetes Bond

The other was purely mental.
My daughter has seen me put an Omnipod on 100 times. She’s even helped me do it. She decorates them by coloring or putting stickers on them.
She would love to be just like Daddy and share this bond with him…..right?
Well, that’s what we were hoping.
The first few times we put a new Pod on, I would do mine just before so that she could see me do it and get comfortable with it.
Six Months Later
We are now over 6 months with the Pod and we absolutely love it. It can still be a battle every so often on putting a new one one, but we know these struggles are going to happen. It simply comes with the territory of having a child with type 1 diabetes.
I will write in a future blog post about our tips for keeping the Omnipod on, how we take it off, how we rotate the sites and many more cool ideas that we have learned over the last 12 months of managing not only my own Type 1 Diabetes, but also our daughter’s.
I hope you are enjoying this content, if so, please leave a comment below or go share the love on Facebook and Instagram.